“We wanted to develop a way to quickly collect mosquitoes and test them, find out where the virus is, and let our operations personnel know so they can exactly target the mosquitoes before it gets to a widespread epidemic,” says Greg White, vector ecologist for the District. “All this is to prevent the spread of disease to humans.”
Southern California’s Coachella Valley extends from the San Bernardino Mountains in the north to the Salton Sea in the south, and for the months of June, July, and August it is over 100 degrees Fahrenheit every day, only falling below 100 when the sun sets. Coachella Valley is home to the resort cities of Palm Springs and Palm Desert, over 120 golf courses, and 95 percent of all the dates grown in the United States, which require tremendous amounts of water to keep fresh, green, and growing. Combine the immense heat with all that water, and you get one thing: a perfect breeding ground for mosquitoes, even in the middle of a desert.
The Mosquito and Vector Control District’s new BSL-3 laboratory is only the latest entry in a long history of arbovirus surveillance. Founded in 1928, the District’s first mission was controlling the local population of eye gnats, at the time creating a huge nuisance also implicated in causing epidemic infections of conjunctivitis. In 1951, the District’s program was expanded to focus on mosquito control.
Preventing the Spread of Disease
The District uses two kinds of traps to catch mosquitoes, the first stage in their arbovirus surveillance. Both traps target only female mosquitoes—as only the females blood feed in order to acquire the protein necessary for laying eggs, only the females can transmit blood-borne pathogens.
The first kind, a CDC-type CO2-baited trap, targets mosquitoes seeking a host to feed on. The trap is loaded with dry ice, which releases CO2 as it sublimates, analogous to human and animal breath. A fan at the top of the trap sucks mosquitoes in as they approach the attracting CO2, holding them within the trap’s chamber until it is collected by researchers.
The second kind, a gravid trap, targets pregnant mosquitoes looking for a place to lay their eggs. The trap is baited with alfalfa-infused water, which may smell bad to humans but is very attractive to mosquitoes. When the mosquitoes approach, once again a fan sucks them in.
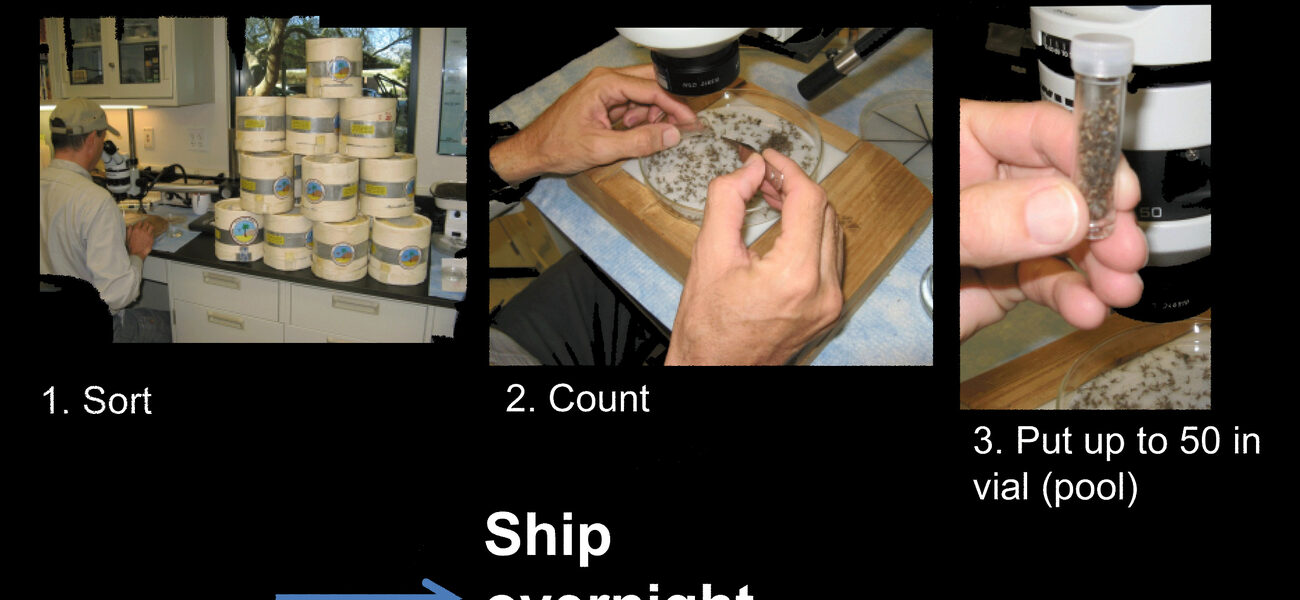
Back in the laboratory, researchers fumigate the mosquitoes with triethylamine, permanently anesthetizing them but keeping them alive—a vital step in order to preserve the possible viral genetic material, which would deteriorate in a dead host. Mosquitoes are counted under a microscope and separated by species; those that are irrelevant to the District’s testing are set aside. The rest are loaded into vials, up to 50 per, and shipped overnight to an external facility for testing.
The path of transmission for an arbovirus begins with mosquito infections before moving on to infections of birds, tree squirrels, horses, and finally humans. However, says White, “the District doesn’t have many tree squirrels, and most horses are vaccinated, and by the time it reaches humans, it is really too late.” Therefore, the District’s second line of defense lies in the study and prevention of avian infections.
The District uses sentinel chickens, usually in flocks of ten, and takes a blood sample every two weeks. If the chickens’ blood contains antibodies to arboviruses, they are being fed upon by local infected mosquitoes. For known arboviruses, such as the West Nile virus, the St. Louis encephalitis virus, and the Western equine encephalitis virus, this is an excellent early detection model.
Avian infection information can come not just from live birds, but also from dead ones, so the state of California runs a hotline for reporting dead birds (and squirrels). If the program reports a fresh dead bird of the right species, the District will collect the bird and ship it to the state for testing.
Expanding Functionality, Reducing Response Times
Tracking the spread of viruses is a painstaking process. If a trap delivers virus-positive mosquitoes, researchers must lay new traps in the region surrounding the first, seeking more positive results in order to track the virus’s vector. But the longer the process of getting test results takes, the more time the virus is given to spread unchecked.
Currently, the District sends its mosquitoes to the Center for Vector-Borne Diseases for testing. The turnaround time for results is two to five days. “We want to test these mosquitoes in-house to give us a turnaround time of only one to two days,” says White. Expanded testing takes five to twelve days from the time of initial trapping. “We want to bring this down to three to four days,” he says. The state takes one to two weeks to return results for dead birds. White says, “We can do that in-house same-day or next-day.”
Not only that, but by outsourcing their tests, the District is beholden to only testing for those diseases they pay to have tested, and only at intervals the external laboratories provide. “If you are only looking for three things, that is all you are going to find,” says White. In-house, the District can perform a wider range of tests, any time they like.
A New Laboratory
“Clearly, having the capability to do in-house testing can reduce the spread of disease,” says Yun Lee, senior laboratory planner for HDR Architecture, which Coachella Valley turned to for performing a feasibility study on expanding their facility. But she highlights a central concern of arbovirus surveillance: “Most of the time they need a Level 2 space, but sometimes they require Level 3.”
Different viruses require different levels of biosafety. For example, according to the BMBL, for the West Nile virus BSL-2 is recommended for processing field-collected mosquito pools, but recommends BSL-3 for manipulations of West Nile virus cultures, experimental animal cultures, and vector studies. While some non-invasive procedures can be performed on dead birds in a BSL-2 (or lower), the BMBL recommends BSL-3 for any dead bird dissection. BSL-3 practices and facilities are recommended for the Western equine encephalitis virus, endemic to the Coachella Valley region, because of its higher risk of aerosolization.
“We decided going to BSL-3 would be a wise decision for both working with dead birds and future studies with viruses, including growing viruses for positive controls, ourselves,” says White. The new laboratory will combine a primarily BSL-2 laboratory with an optional BSL-3 space, to be used whenever testing deems it necessary.
By Braden T Curtis
This report is based on a presentation by Lee and White at Tradeline’s 2013 International Conference on Biocontainment Facilities.