With its new Clinics and Surgery Center, University of Minnesota Health has taken a bold new patient-centered, technology-enhanced approach to clinical care. Patients are greeted by a concierge instead of waiting at a reception desk, and are guided through their visit by a step-by-step itinerary; and their progress is monitored through an RFID-chipped badge they wear for the duration of the visit. The building has improved the way care is delivered, while at the same time improving space utilization.
The 342,000-sf, five-floor facility opened in 2016, serving 37 adult specialties with a wide array of services, including:
- Primary care
- Clinics for cancer, cardiology, endocrinology, gastroenterology, neurosurgery, orthopedics, otolaryngology, pain management, pulmonology, rheumatology, transplant, surgical specialties, ENT, urology, hepatology, nephrology, infectious diseases, solid organ transplant, neurology, physical medicine and rehab, dermatology and derm surgery, cardiology, pulmonary, signature health and wellness, and acute injury.
- Diagnostic and treatment suites
- Lab and imaging center
- Pharmacy
- Multiple ambulatory surgery and procedure suites
The first floor features imaging, lab, and retail pharmacy space. The cancer and advanced treatment centers occupy the second floor, and the third comprises medical specialty clinics. On the fourth floor are surgical clinics, and the fifth floor houses an executive health program, procedure center, and ambulatory surgery center, a service not available in the previous site.
The $165 million facility replaces a nine-story building hampered by a challenging layout, with poor space allocation, limited adjacencies, and an entrance that was difficult to access. The building was also inefficient, with a space utilization of only 40 percent.
“Our vision was to develop a building that had innovative healthcare models implemented by interprofessional teams,” says Marlene Pechan, vice president of clinical operations for University of Minnesota Health. “Our patient experience had to be extraordinary.”
Not Your Typical Doctor’s Office
The new center doesn’t look or operate like a typical medical office. When a patient contacts the centralized call center to schedule an appointment, they are asked to sign up for the MyChart electronic health record and communication service, and are walked through the process on the phone. Patients then receive information on-line, as well as forms and health history questionnaires to complete and return prior to the visit. This allows the care team to be prepared for the visit, and reduces patient time in the center.
Patients also receive an itinerary, either electronically or on paper, detailing the components of their upcoming visit. When they arrive, they pay $6 for valet parking, a flat fee regardless of the length of their visit. Upon entering the building, they are greeted in the lobby, not at a reception desk, but by a staff concierge with a tablet, who helps with wayfinding, electronic signatures as needed, and digital payment processing. All patients, doctors, nurses, and staff wear “Care Connect” badges equipped with RFID technology, so they can be located at any time. Physicians who need assistance during an exam can press a button on their badge to call for a staff member.
The RFID technology also improves exam room efficiency, by allowing physicians to use the first available space rather than a room assigned to them. Sensors in the badges are read by sensors in the exam rooms, and their status is displayed on a digital monitor. Green indicates a room is available, yellow that a patient is inside, and red that the room needs to be cleaned. Each patient’s status is monitored, as well, and an electronic notation is made automatically if they have been waiting in the lobby for 15 minutes, or left alone in an exam room for 10 minutes. That signals a staff member to approach the patient, acknowledge the delay, and seek information from the care team about when the patient will be seen.
“We ask patients if we can take their photo, explaining that with their picture and the RFID badge, we know what they look like and where they are sitting, so we no longer have to call their name when it’s time to go to the exam room,” says Pechan. Instead, a staff member can find them and quietly approach them to say they are ready to be seen, then escort them to the correct location.
At the end of each visit, patients have the option to fill out a comment card, which is reviewed by staff daily. Staff follow up on every comment, positive or negative, by contacting the patient.
The clinic offers virtual options, too. E-visits use the MyChart system to query patients about their condition. A healthcare team then determines next steps, whether a patient should be treated with home care or by a physician in an office visit. Televisits allow physicians to monitor patients via medical devices and peripherals that transmit data to the patient’s digital record. Secure video feeds allow doctors and patients to interact and assess minor conditions without a live visit.
New Approach to Building Design
The new building abandons the traditional exam room allocation, where physicians were assigned a number of designated rooms for exclusive use. The new facility houses 170 uniformly designed 110-sf exam rooms, more than 100 fewer than in the old building.
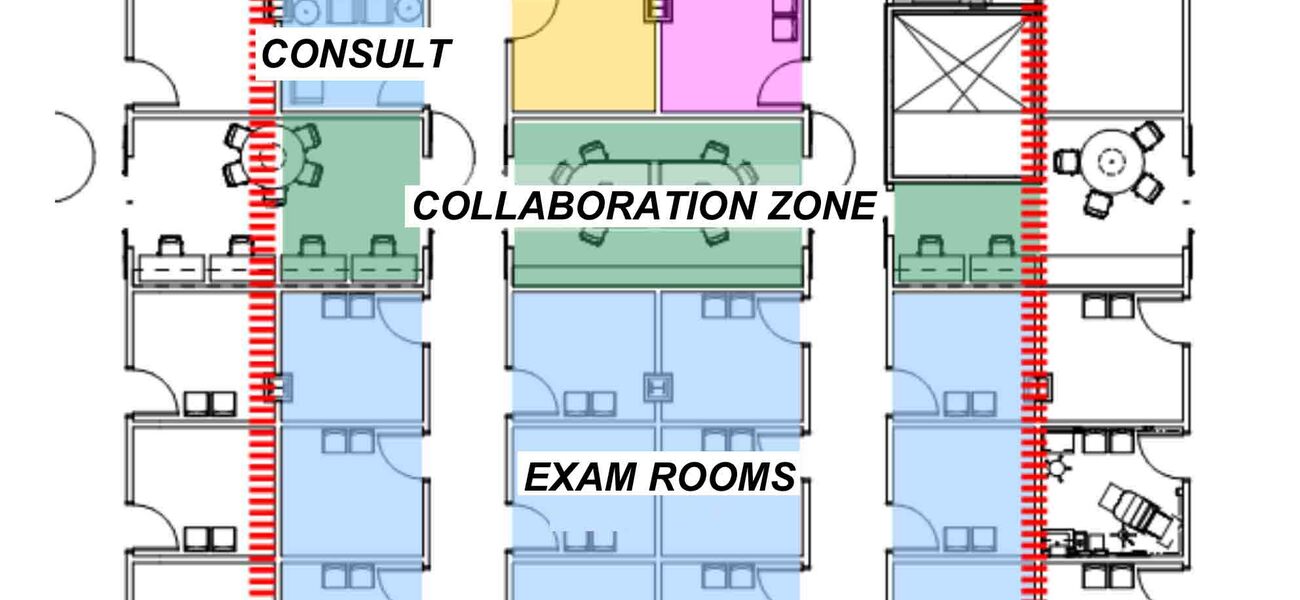
A modular, flexible design is key to the building’s space efficiency, and makes it adaptable to change. A typical module includes a waiting and intake space, where vital signs are taken before patients are escorted to one of the 12 exam rooms. Procedure rooms and consult rooms are in the back of the module. The 10 operating rooms include state-of-the-art equipment and one unusual feature: windows, installed at the request of the surgeons.
One of the hallmarks of the new building is the collaboration space, running the periphery of the building behind the exam rooms. It allows physicians and staff to move through the interior of clinic space and more easily interact than was possible in the former building. Specialties that typically consult with one another are located in close proximity, so teams can easily confer and collaborate.
There are no offices in the facility to further increase efficiency. Instead, staff members use “touchdown spaces,” which are again uniformly designed and not assigned to individuals. Electronic medical records are accessible at any computer terminal.
As a result, the move to the new building required a significant reduction in paper. “That was quite a journey to go on,” says Pechan. “While it was tempting to bring paper and personal belongings to a touchdown space, staff were encouraged to engage in the 5S process and convert paper to an electronic solution whenever possible, and to store personal pictures on their phones.”
The few papers that remain are placed in cubby spaces, leaving the 220 touchdown workspaces clean at the end of each day. There are also a limited number of private touchdown spaces for private meetings or sensitive discussions.
Some of these changes were not readily welcomed. For example, several of the staff members who previously worked behind reception desks were concerned about being on their feet all day as concierge team members. Accommodations have been made to ensure a comfortable work situation, but some employees have left the company because they did not like the changes.
The locator system also met some early resistance.
“Some of our doctors and nurses were concerned we would be watching them all the time,” says Pechan. “That’s not our intent. Through our training, we assured our providers and staff we would use the data only to monitor and improve workflows, bottlenecks, wait times, and patient experience.”
And retrieving those expensive badges from patients at the end of a visit can be difficult, especially in Minnesota winters when visitors bundle up to leave. Pechan reports that valets now check with patients to ask about the badges. If someone ends up taking one home, the patient is notified to simply drop it in a post office box, as the center’s address is imprinted on the back of the badge and the post office returns it.
Developing a Patient-Centric Experience
The goal of the new facility was to make it more accessible to patients. Hours of operation expanded from 8 a.m.-4:30 p.m. to 7 a.m.-7 p.m. weekdays, and Saturday morning hours were added to better accommodate patients’ schedules.
Most of the clinics at the center now use a free-standing billing model, decreasing costs to patients. Previously, the practice used a provider-based billing model, which is commonly used for hospital-owned sites, whereby patients receive two bills, one for the facility charge and the other for the medical services provided. Now patients receive only one significantly smaller bill, resulting in reduced revenue for the practice. The change was made to better serve patients and remain competitive in the marketplace, says Pechan, and was financially possible because of the increased efficiencies.
Growth in new patients at the free-standing clinics increased from 7 percent annually to 20 percent. Surgeries grew by 43 percent through June 2017, driven by the addition of new procedures and the use of the ambulatory surgery unit. At the same time, costs per insurance claim are down 22 percent.
Officials believe that they saved $60 million to $70 million in construction costs due to the process improvements that allowed for a smaller building footprint. The building is roughly one third smaller, but accommodates one third more activity, with the efficient design and expanded hours of operation.
The Care Connect system also provides detailed space utilization data, which demonstrates that the reduction in exam rooms is justified, and can also be used to inform future building modifications. Pechan says the team is now looking at the staffing models within the building to further reduce cost and optimize the role of nurses. They also are looking into increasing the number of advanced practice providers to see return patients, allowing physicians to see more new patients.
By Kevin Wesley