The Clinical Cell and Vaccine Production Facility (CVPF) at the Hospital of the University of Pennsylvania is designed to facilitate a bench-to-bedside approach, where the clinical materials to treat disease are manufactured and administered within the hospital using cells from the patient’s own body. The project has achieved international recognition for its unique potential for optimizing patient care and for its success treating human immunodeficiency virus (HIV) and cancer. The challenge was to renovate the 50-plus-year-old facility in order to meet strict Food and Drug Administration (FDA) standards for good manufacturing practices (GMP), as well as guidelines governing drug manufacture and distribution, in an effort to expand cell processing capabilities to treat more patients.
“We were essentially building a pharmaceutical establishment within a hospital, with all the regulations that requires,” says Don Siegel, M.D., Ph.D., director of the division of transfusion medicine and therapeutic pathology for the hospital system.
Cell therapy uses a patient’s own cells to create a vaccine to treat specific diseases, rather than using conventional, mass-produced medicine, like chemotherapy drugs for cancer. Patients enter the hospital on an outpatient basis and are connected for two hours to an apheresis machine (similar in appearance to a kidney dialysis machine) that removes white blood cells from their blood. In the lab, researchers manipulate the cells using DNA to create new cells that recognize and kill the disease. These new cells are grown in the lab, and about two weeks later, are injected back into the patient. In theory, the process can make cells that recognize and destroy any type of cancer. So far, it has worked successfully for many patients with chronic lymphocytic leukemia (CLL), and acute lymphoblastic leukemia (ALL). The goal is to develop this approach for many other types of disorders, including infectious diseases like HIV.
“This facility allows us to create a new kind of drug therapy in the sense that each drug is made from a person’s own cells. Your own body’s cells fight your disease. It’s very personal, because the cells work only in one person. You could potentially have 100,000 patients and 100,000 different drugs,” says Siegel.
Project History
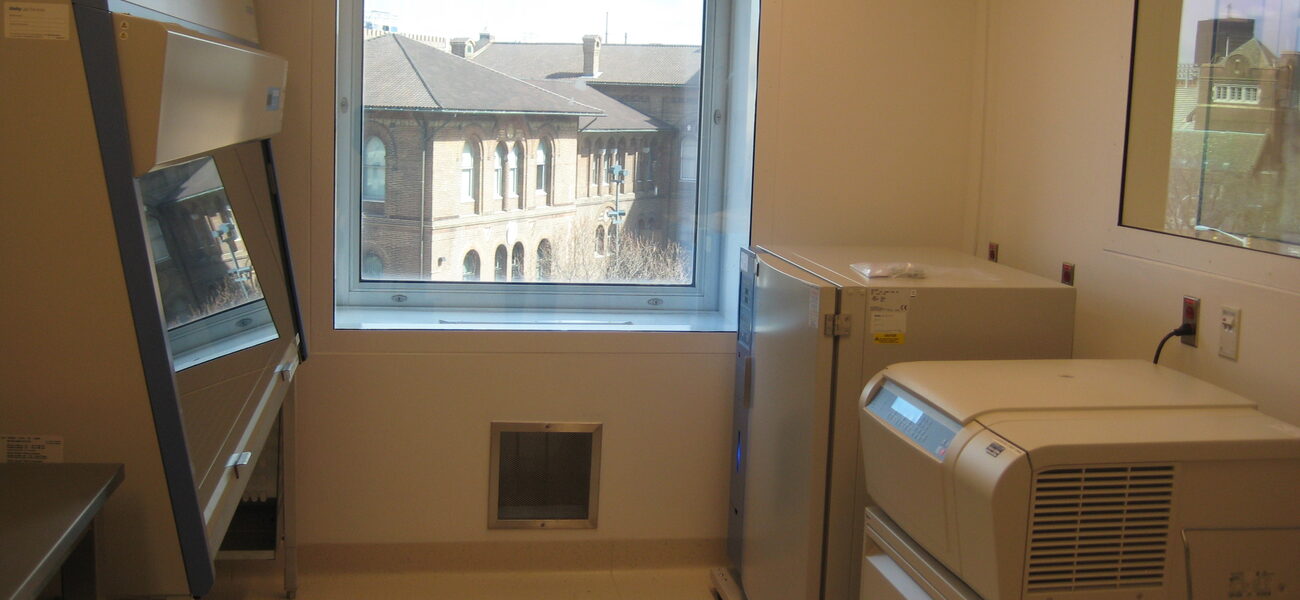
Hospital researchers initially used a 300-sf lab for cell manufacturing, moving in 2005 to a lab of 1,800 sf, which was repurposed to GMP standards but had a very limited capacity. The newly renovated CVPF space occupies a total of 14,700 sf, with 2,500 sf of classified production space. The renovations are on the third floor of the hospital, above the neurology clinic and below the operating rooms. The space includes seven patient cell processing rooms, five more than previously. Since there is the potential risk of cross-contamination among patient cell products, separate processing rooms for each patient’s cell culture are necessary.
“Typically, the concern would be cross-contamination between different drugs manufactured in a facility, but in this case, each drug is specific to a given patient, and when you are working with multiple patient products, safety concerns are multiplied,” says Siegel.
At the same time as the CVPF renovation, the hospital expanded a blood stem cell lab for routine cell processing for bone marrow transplantation. While these areas were built at the same time, and both deal with blood products, they require very different strategies related to GMP, mainly regarding ventilation and airflow. “They are co-located and have some synergies, but keeping the spaces separate became a key driver in laying out the overall available space,” says Doug Bradley, project manager for Jacobs, the principal design firm for the renovation. Research staff and design staff met weekly for more than a year to plan the renovation.
Aseptic Conditions
The CVPF area is designed to meet FDA standards for aseptic processing for sterile products containing no living organisms. This is the highest level of cleanliness defined by the FDA, generally applied to injectable and ophthalmic drugs, and has strict guidelines governing air-locks and gowning, filtration, pressurization and flow, surface cleanability, containment, and segregation, with established procedures for handling waste and materials.
“We knew how clean we needed the space to be. However, it’s one thing to build a lab like this and another to build it inside an existing hospital,” says Siegel.
FDA regulations require ISO standards, or particle count, that must be maintained in the CVPF. Adjacent to the main lab are changing rooms, where lab workers don gowns and gloves and generally disinfect, then exit through an airlock into another clean area rated ISO 8. A hallway leads to the seven patient processing rooms, each rated ISO 7. Inside each of these rooms, where cell containers will be opened, is an aseptic work area (rated ISO 5) equipped with a laminar flow hood with fewer than 100 particles of 0.1 microns or greater in a cubic meter of air.
Part of creating a sterile environment is eliminating contaminants, like microorganisms/endotoxins and particles, which could enter through the air handling system, on equipment, materials, or humans. The biggest risk to the aseptic process is people coming into the space from less-controlled areas.
“A major driver in aseptic design is dealing with the particles and bacteria involved with operators,” says Bradley. For example, there are more than 1 million bacteria-forming microbes on 1 square centimeter of scalp. Bacteria on 1.75 square centimeters of skin surface can be twice that, and the outer layer of human skin is replaced every five days, shedding particles in the process at the rate of about 10,000 particles per day.
Engineering Challenges
The goals for the design were to meet FDA aseptic standards and maximize the available space within the hospital’s 14-foot floor-to-floor height. Due to space constraints, all mechanical systems related to air handling are located on an adjacent low roof area in a pre-fabricated enclosure. This air handling enclosure also has a walk-in service corridor and houses the purified water system. The roof is reinforced to accommodate the increased load. About 80,000 pounds of connecting ductwork provide the air changes and systems necessary for GMP production, including an exhaust stack attached to the side of an adjacent 14-story building.
“In a normal scenario, you would create a full mechanical floor above the production area,” says Bradley. “It was a very constricted project area within which to try to develop a highly technical production facility. With such a tight floor-to-floor height, every inch mattered.” To avoid disrupting daily hospital operations, a crane lifted new equipment from outside the building, at a cost of $200,000 to $300,000 per day.
FDA regulations for air handling and pressurization in GMP areas require more stringent control, validation, and change control than anywhere else on the floor or in the rest of the hospital. Thus, GMP and non-GMP areas have separate air and building management systems (BMS) controls. They share an exhaust system, however, as none of the air is re-circulated. The GMP area is required to have air changes of 14,000 cubic feet per minute. These levels are even higher in areas where cells are manipulated.
“Keeping these systems separate was entirely due to the rigors of validation protocols. These are not requirements you want to force on the hospital systems,” says Bradley. “We often had the conflict between what is required for a hospital operation, and what is required for GMP production.” To maintain pressurization, the CVPF is fitted with airlocks, in concert with cascading pressurization from most- to least-clean areas. “We had airlocks beyond what you might normally have to keep our facility isolated from the general corridors,” says Bradley.
The complexities of meeting mechanical requirements, installing equipment, the high level of cleanliness, and the rigors of creating a sterile area within the limitations of a hospital make this expensive space, about $10 million for the Clinical Cell Vaccine Production portion of the project. “From a design standpoint, it was an incredible accomplishment,” says Siegel. “There are very few labs in the country doing this type of work, and to build one within a busy hospital is a remarkable achievement. In terms of design, as well as cost, it would have been easier and less expensive to build such a facility off campus, but in this case, the overriding goal was to improve patient care by having cell processing adjacent to where patients have their cells initially collected and eventually re-infused.”
The University has a licensing agreement to commercialize the process and create designated treatment sites throughout the United States, which would make this treatment more widely available.
By Mary Beth Rohde
The report is based on a presentation at Tradeline’s Academic Medical and Health Science Centers 2013 conference.