Bringing biosafety laboratories into compliance with the BMBL 5th Edition’s “zero airflow reversal” clause requires assessing risk appropriately, analyzing the impact of a pressure envelope on the facility, installing appropriate ventilation and control systems, and implementing new control strategies for practical testing.
It is critical to assess not only the laboratory in question, but how the upgrade process may affect the entire facility, says Valerie Klengson, senior national sales manager of Siemens Life Science Solutions. “You have to understand the total business impact associated with this guideline,” she says. “You could have a vivarium or other critical space in the basement that gets affected. Depending on your ventilation system, you could have an entire floor shutdown requirement, or even an entire building shutdown,” and not just a temporary closure of the lab being upgraded. These factors are fundamentally important to the ultimate considerations of any upgrade project: time, budget, and cost.
Appropriate risk assessment is vital before proceeding with any implementation: What science will be taking place in the laboratory? What are the laboratory’s modes of operation? What are the pass/fail criteria of evaluations? All these questions must be answered, and any such assessment should involve all the facility’s stakeholders as early in the process as possible, so that everyone moves forward in the same direction.
Additionally, Klengson emphasizes the importance of involving an experienced commissioning agent in the upgrade process. “If you don’t,” she says, “you need to make sure that your design engineers and control contractors have BSL-3 upgrade experience.”
The Pressure Envelope
In any facility, there is a direct correlation between the negative pressure required to maintain inward directional airflow and the tightness of the space. Labs in containment are built to permit inward airflow through tightly controlled points and to eliminate uncontrolled leaks. In other words, Klengson says, “If you want any chance whatsoever of getting a zero flow reversal, you really need to button up the leakage space.”
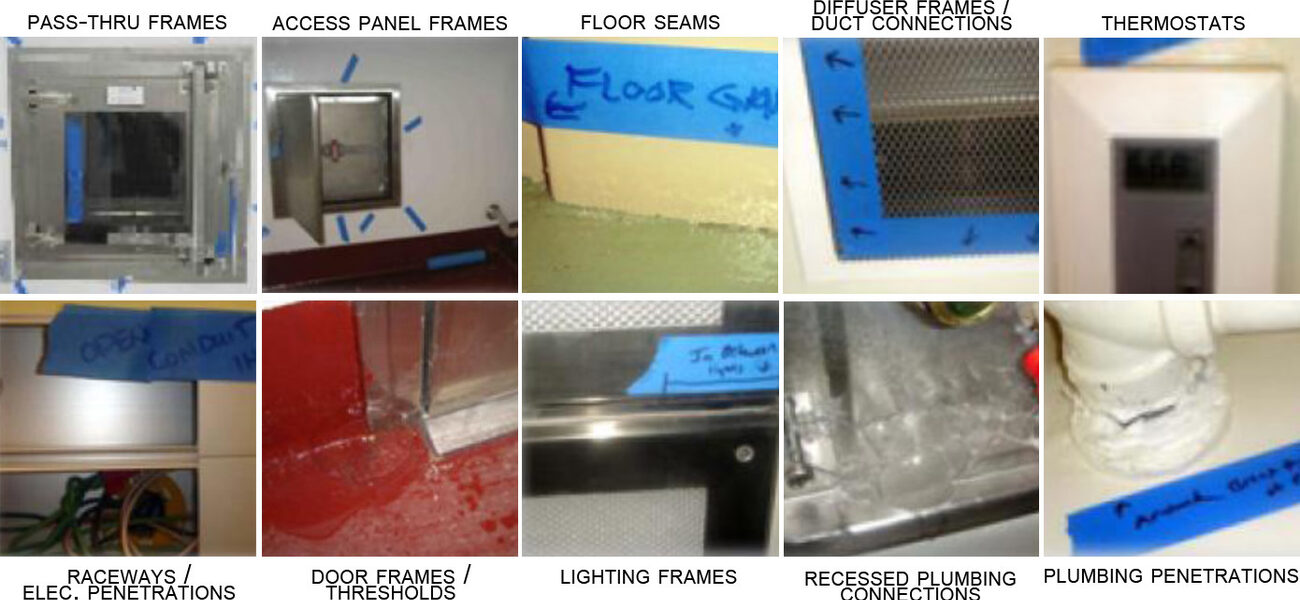
Consider a room leakage test to identify and repair leakage points, which are commonly found in:
- pass-through frames
- access panel frames
- floor seams
- raceway and electrical penetrations
- door frames and thresholds
- plumbing penetrations
- thermostats
- diffuser frames and duct connections
- lighting frames
- recessed plumbing connections
“You have to get your caulk out,” says Klengson.
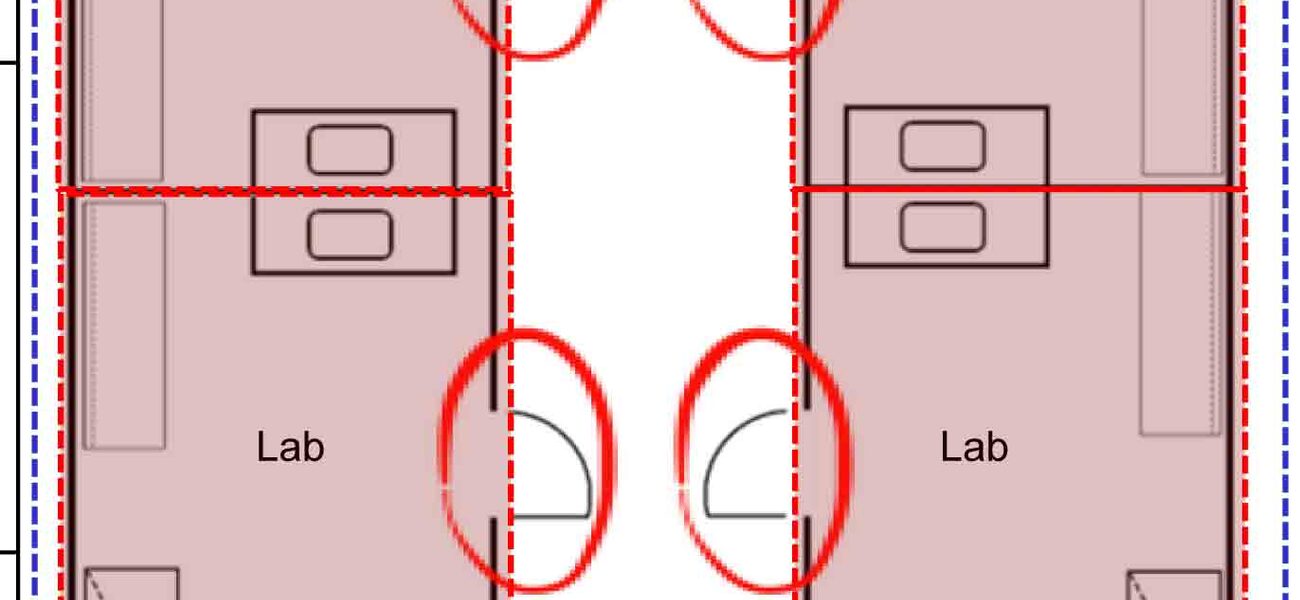
The next-most-important consideration to preventing leaks is defining the laboratory’s containment boundary. Notably, under the current regulations (the Select Agent Rule), any such containment area should include an anteroom within its boundary.
The CDC is concerned with excursions into the public corridor and between labs—anything outside the outermost anteroom. This does not include zero flow reversal across interior doorways in a multi-suite lab, however. “That is very different,” says Klengson. “A facility may require zero flow across interior lab spaces if it affects the research. Note that achieving this could add months of commissioning time, as opposed to achieving it only across the anteroom leading to the public corridor, and must be identified at the onset of the process. However, it can be accomplished.”
Ventilation and Control
Upgrading the lab may require an upgrade in actuators, as well.
“Historically, acceptable pressure control of BSL-3s could readily be achieved using standard actuation,” says Klengson. These laboratories typically involve constant volume scenarios where actuators need only respond to minor adjustments and temperature changes. In general, they are steady operations. Unfortunately, in attempting to achieve zero flow reversal, standard actuators may no longer meet requirements.
To achieve zero flow reversal, the laboratory may require fast actuation. Unlike traditional commercial buildings, for which “fast actuation” generally means operations of 90 seconds or less, zero flow reversal fast actuation requires an operation in under two seconds full stroke. Understandably, fast actuators have a greater power requirement than their standard counterparts.
Another traditional piece of equipment that may be in need of replacement is the application-specific controller. These controllers, with their programming already built in, are cost-effective methods of performing certain functions. However, particularly in multi-suite laboratories, where pressurization may need to be controlled across multiple interior boundaries, laboratories may want to upgrade to a fully programmable field panel.
Consider uninterruptible power sources, as well. “Even if you are on emergency power, the blip when you switch from standard to emergency power could create flow reversal,” says Klengson. “You are going to want to put all your controllers and actuators serving those spaces on UPS.” This arrangement is already a requirement in the NIH design resource manual.
Does your laboratory have bioseal dampers? Chances are, you will have to install bioseal dampers if you don’t already have them, says Klengson. While historically these dampers were used primarily in decontamination processes, they are quickly becoming a part of the sequence of operations to close off air supplies in failure events. Bioseal dampers will necessitate the installation of relief dampers, as well, because even variable-speed fans cannot react fast enough to protect the integrity of the ducts.
Optimally, biosafety laboratories have dedicated supply and dedicated exhaust systems, but in the more likely scenario that your laboratory shares HVAC systems with other elements of your facility, you may need to install isolation dampers. Keep in mind that fast actuation is needed here, as well, on both the room and fan levels.
New Control Strategies
A very real consequence due to the potential overcompensation to achieve zero air outflow is potential damage to laboratories during testing. Vacuum conditions caused by a cut-off air supply and continuing air exhaust can do everything from pulling off caulking to tearing down ceilings (traditionally the structurally weakest portion of a laboratory). How can testers adjust their strategies to the new requirements?
“One method that we used was what we would call a ‘distress mode,’” says Gary McKelvey, service operations manager for Siemens. “We place a pressure sensor at the intake of the exhaust fans and as soon as it senses a lowering of pressure, it starts controlling the supply at a lower CFM.” This starts preventing flow reversal at the supply and exhaust fan levels, by anticipating a loss of exhausting and immediately reducing the supply.
However, this can quickly create a high negative pressure. The solution begins with bi-directional airflow tracking—monitoring both the inflow and outflow of air through the supply and exhaust at the room level. From there, you can track not simply air supply and exhaust, but the differential between the two.
For example, take a typical lab with a total exhaust of 1,000 CFM, and a supply of 800 CFM. The 200 CFM differential there will maintain the room’s negative pressure. If the room’s supply is at 0 CFM, therefore, an exhaust of 200 CFM (or another safe negative differential setpoint that is tested during the commissioning process) will still maintain negative pressure, without the disastrous vacuum conditions that lead not only to laboratory destruction, but also vacuum-sealed doors, potentially trapping researchers within a contaminated lab. Upon supply startup, the system continues to prevent flow reversal by bringing up exhaust at the same 200 CFM differential rate.
These two methods form a comprehensive approach for safe laboratory control and testing, while meeting the BMBL-5 requirements. “We compare how the air handlers and exhaust fans work together. Using distress mode, we try to anticipate any kind of failure in the exhaust system. At the room level, we use bi-directional airflow to maintain zero flow,” says McKelvey.
By Braden T Curtis
This report is based on a presentation by Klengson and McKelvey at Tradeline’s 2013 International Conference on Biocontainment Facilities.