As part of a master planning initiative, the University of the Sciences in Philadelphia used survey tools to examine how faculty, staff, and students collaborate; how they use the campus; and how University facilities compare to other institutions. More challenging was finding a way to express qualitative data in a quantitative way, and share this data with campus leadership to inform planning and design decisions.
“When I first embarked on doing this survey myself, as a faculty member and an administrator, a lot of stuff was somewhat intuitive. But when we saw the results, it told a very powerful story,” says Cathy Poon, associate dean of IPE and chair, University of the Sciences Department of Pharmacy Practice and Administration. “I think it sold it to the organization and our leadership to let us move forward in a manner that made more sense with the data, not just what we thought it would be.”
The results call for reorganizing space to create adjacencies between academic medical programs, more hands-on learning with healthcare simulation areas, flexible lab and classroom space, and more opportunities for departments to share space and collaborate.
Gathering Data
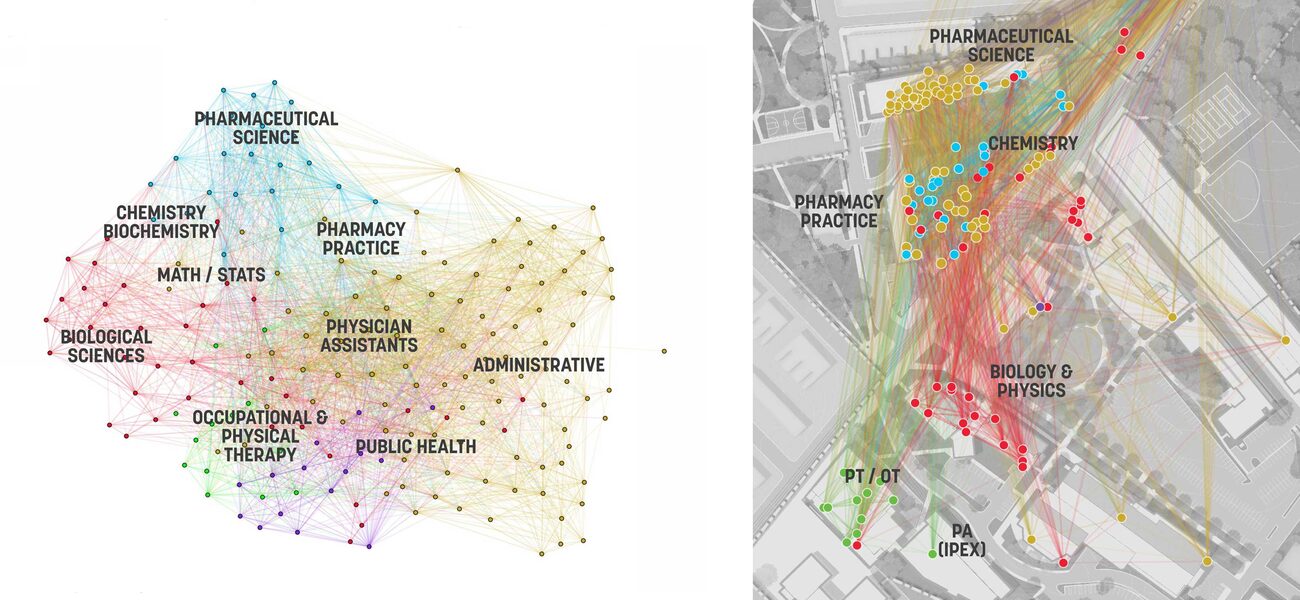
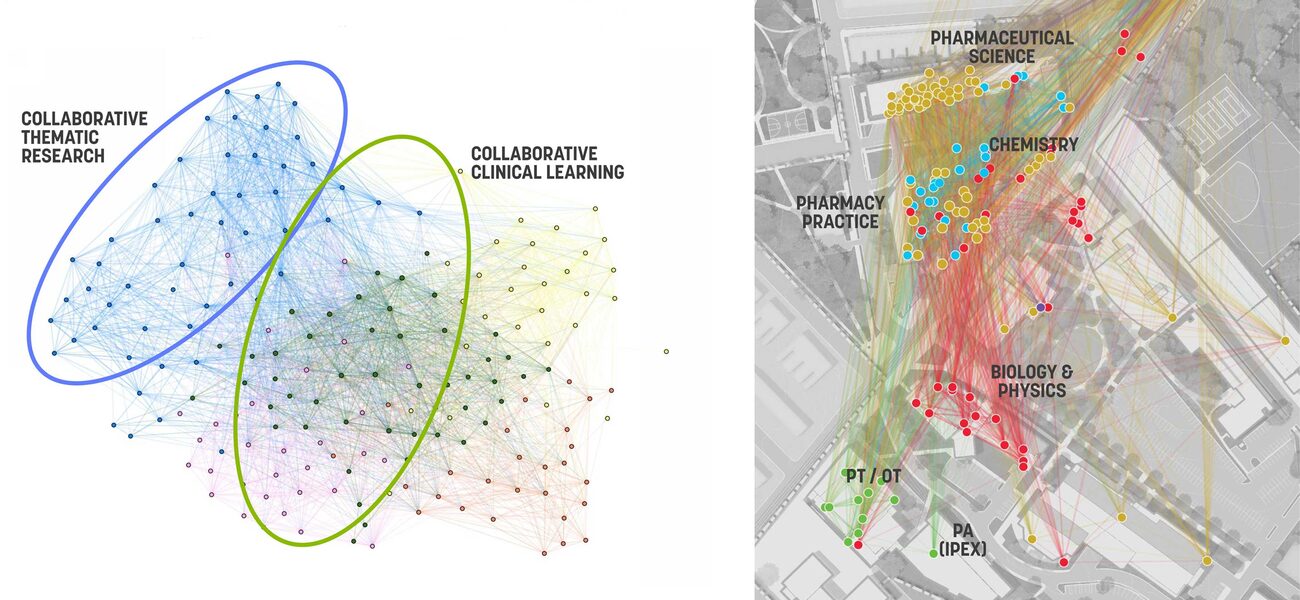
The uniquely designed surveys provide an array of information about the social nature of a campus and its facilities to create an objective view of reality, according to Tom Simister, an architect and senior associate at the design firm, Sasaki, which created the survey tools. For instance, a Collaboration Survey asks faculty and staff in biological science, pharmaceutical science, chemistry/biochemistry, pharmacy practice, physician assistants, public health, occupational/physical therapy to rank in order of high-medium-low, who their collaborators are now, and with whom they aspire to collaborate. The results can be viewed by a community group or department. “It visualizes the social interactions between groups, so we can see how fragmentation is occurring, and also what the desired adjacencies are. If you are looking at research themes, or better alignment between departments and programs, this is a very powerful picture to present to leadership about ways to make institutional change on campus,” says Simister.
Used in early planning stages, the MyCampus Survey asks staff, faculty, and students to use drag-and-drop icons to show how they use the campus and indicate what works and what doesn’t: Green is thumbs up, yellow is neutral, and red is thumbs down. Users can add comments, and highlight problem areas, such as streets with limited parking, buildings that lack study space or technology, and areas that feel unsafe. “We do this on a campus level and at a building level so we can see the critical flows and the conflicts. This kind of tool makes deeper analysis possible,” says Simister. Faculty and staff focused their comments on physical or organizational improvements on campus. “When the administration realized that, for undergraduate students, the campus boundary overlaid with concerns about walking paths, it solidified the decision to acquire an adjacent school site and develop that for residential housing,” says Simister.
Suitability Evaluation is a planning tool for computational analysis of building suitability, comparing University buildings to Sasaki’s database of similar university facilities across the country, using criteria such as floor-to-floor height, structural grid, window pattern, overall building width, partition flexibility, building system capacity, roof/basement capacity, loading/handling capacity, and historic classification. The information aids facilities decisions about whether to demolish or divest a property, convert or change the use—such as for labs, residences, or offices—or stay the course. “We can get on the same page about what the building’s highest and best use is long term,” says Simister.
Setting up the Space
Based on survey results, and expected changes in accreditation that indicate specific experiences for each learner, the first phase of the master plan focuses on 18,000 sf of third-floor shell space in the 57,000-sf Integrated Professional Education Complex (IPEX). The space is being organized to create adjacencies between academic medical programs, and co-locate occupational therapy, pharmacy, physical therapy, and physician assistant education. There will be more simulation areas for hands-on learning, flexible lab and classroom space to accommodate various group sizes, and more opportunities for these departments to share space and collaborate. The renovation, expected to be finished this fall, will have an inpatient pharmacy to simulate a hospital cleanroom; a community pharmacy to simulate the retail model of patient/pharmacist consultation, and clinical care/patient care rooms. “We lacked space for hands-on teaching and simulation. Short-term, we needed to accommodate our existing curriculum, but we also want to accommodate future accreditation standards, and achieve both goals with the new space,” says Poon.
In making decisions about optimal teaching space, it’s helpful to look at both survey data and accreditation standards. “We find that benchmarks are of limited use,” says Simister. For instance, accreditation is trending toward a required amount of inter-professional experience, which supports decisions to provide both simulation space and collaborative opportunities. Space programming information comes from meeting with faculty groups by academic program and creating a spreadsheet based how many sessions of each kind of experience or class they teach, how long each lasts, how many students participate, and whether breakout groups and hands-on activities are involved.
“Rather than talking about schedules and numbers of rooms, we need to talk about how many hours does each learner need per year per type of experience?” says Jane Kleinman, RN, MAOM (Master of Arts in Organizational Management), Director of Health Sciences and Experiential Education at Sasaki. Kleinman advocates looking at the trends from an accreditation and pedagogical standpoint, and also based on discussions with clinical partners. “Instead of saying, ‘I want X number of new rooms,’ we are looking at how many, of what type rooms we need to support the curriculum and overall goals. It is an ongoing, dynamic process, where we look at the best possible use of the type of spaces available,” says Kleinman. “If we are talking about classroom space, we think about who else might use it. Based on utilization studies we can understand the use and the flow to make better decisions.”
For the IPEX renovation, every room has three possible uses: instruction, skills practice, and study or meeting space. Room dividers, and moveable tables and chairs make it quick to change from a 200-student lecture to 50-student groups. Patient care rooms can be used for clinic visit simulations with some simple changes. Rather than taking up space with built-in storage, everything is portable and mobile, so materials for virtually any type of activity can roll from one room to another. “In many rooms, the only thing built in is the sink,” says Kleinman. Using lockable, rolling carts set up for specific skills and tasks makes it easier for support staff to quickly change the room; every space can flex rapidly into something else. The flexible floor plan makes it easier for PT, OT, PA, and pharmacy to share space, and work together as they would in a real hospital setting.
Flipping and Spiraling the Curriculum
The renovations support changing teaching and learning styles. Poon describes “flipping” the curriculum to give students alternate ways to access information, such as using online study tools and videos along with reading or classroom activities. Students are more likely these days to be visual learners, comfortable with podcasts and YouTube, who want to access information online and outside traditional class times. “We flip the curriculum so knowledge transfer can happen outside the classroom, even at 2 a.m., and students come class ready to apply the information and synthesize their learning,” says Poon.
In a similar manner, “spiraling” is a learning process that sends students out to immersion simulations, then to real life patients, then back to the classroom for a lecture or discussion, and repeats the cycle for each new skill. In this way, students move forward armed with knowledge from previous experience. Students may cycle through a two-hour or four-hour session where they start out in a big group, then move into different-sized groups for collaborative activities, with some spiraling off to work on skills, and others going to immersion or simulation activities.
“Everybody goes through this continuum of learning, all within the same session. It’s a unique challenge, and requires unique space,” says Kleinman.
By Mary Beth Rohde