Institutions that educate medical professionals are building an increasing number of simulation centers in response to the need for more hands-on, interdisciplinary, real-life training scenarios. Although these facilities can generate revenue, the expense of the equipment and related costs make it difficult to be profitable. But, with the use of creative design strategies, institutions can improve utilization and generate income.
Testing and accrediting agencies now allow simulation to help students prepare for exams and to fill in training gaps, because it’s impossible to predict what types and numbers of real cases medical school students will encounter during their four-year curriculum, says Colleen O’Connor Grochowski, associate dean for curricular affairs at Duke University School of Medicine.
“Now, instead of ‘seeing one, doing one, teaching one,’ students can actually see one, do one, do another, do another, do another, until they achieve competence,” says Grochowski, “and then do one on the live patient who, decades ago, was their dress rehearsal the first time through. We can accelerate their learning curve.”
Several reports in the 1990s focused on medical errors and their effects on patient safety, she explains. Communication was cited as a root cause in about 70 percent of the errors that resulted in deaths.
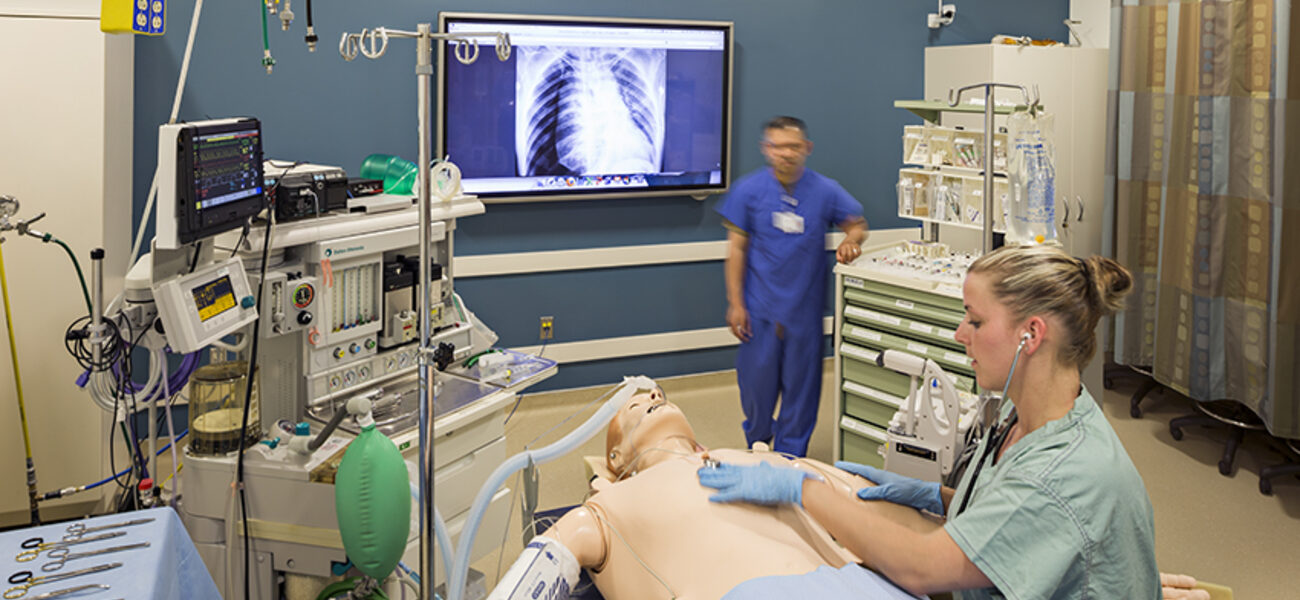
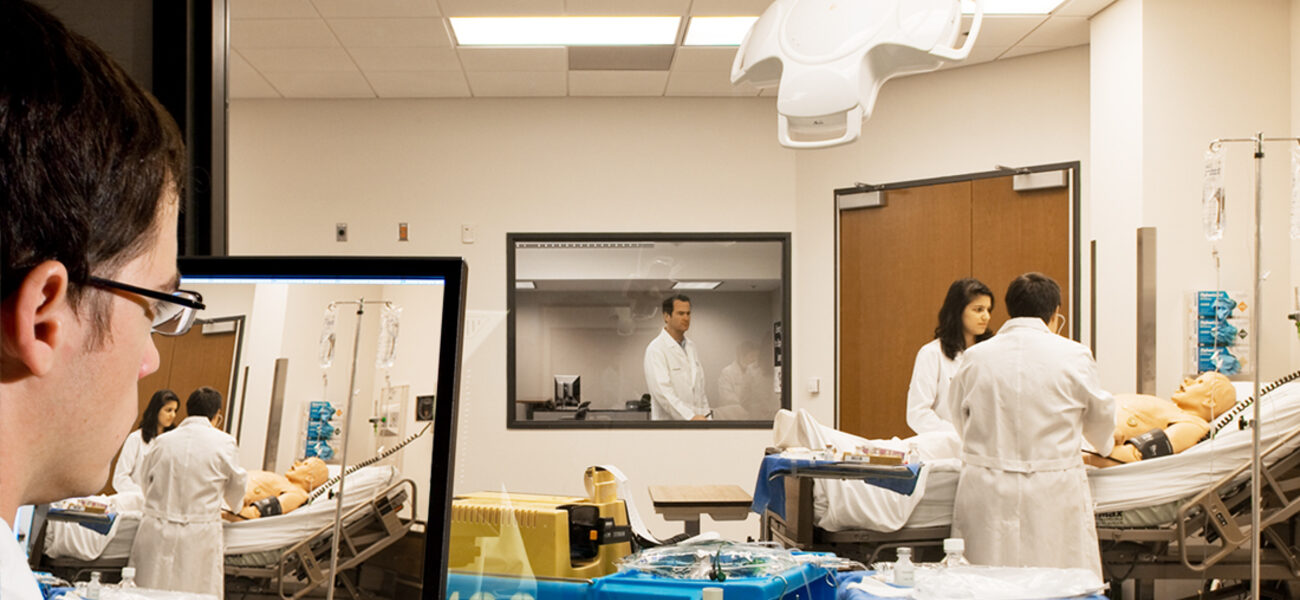
To combat this problem, the educational community began focusing on healthcare training that provides experience working in interdisciplinary teams, with more practicing of the skills health professionals need to acquire and demonstrate. Simulation has evolved from the simple mouth-to-mouth resuscitation training mannequin from the 1960s, to the use of lifelike mannequins and actors trained to play patients.
Simulation is playing an increasing role in graduate medical education, continuing medical education, maintenance, and certification, she adds. Many hospitals are building simulation centers within their own facilities.
“I believe the increase or the evolution of simulation is the next great revolution in medical education,” she says.
Planning Interdisciplinary Simulation Centers
It’s important to keep in mind that simulation facilities will probably not make a profit, says Mary Jo Olenick, a principal with The S/L/A/M Collaborative, a planning and design firm that works on higher education and medical education facilities across the United States.
“People expect these can be money-makers, but the equipment is expensive, you have to staff them, and if you are going to serve the medical education community, there are going to be blackout times (when the facilities are unavailable),” she says. “Even charging people to use it, a simulation center can’t generate enough time to make a profit.
“They are valuable from an education/outcome point of view and community impact. If you use your space wisely, you at least can get the maximum utility and minimize your costs.”
It’s also important to understand the difference between a simulation “program” versus a “center.” As learner experience and desired outcomes expand, the cost, complexity, and need for flexibility increases.
“If we are just educating medical students, that is a program. If we are making a place to put all the program pieces together, that is a center,” explains Olenick.
As changes in healthcare delivery have driven dramatic changes in hospitals, more hospitals are building new facilities and converting old hospital floors and wings into simulation centers. However, this approach can require some compromises in layout, which can impact utilization and staffing levels. The cost of renovation may be less than new construction, but longterm operating costs could be higher, she says.
Future expansion is also an important consideration. “If institutions build a locked-in center, they have no place to expand. So how we put ‘soft space’—space that is easily converted or easily relocated—around these simulation centers becomes an important issue. You need to think about master planning your simulation center as you begin to implement it. Chances are you are going to want or need to expand.”
Overall size depends upon whether the simulation center will focus solely on medical school training or involve community professionals, and other factors such as location (accessibility) in the community, says Olenick.
A benchmarking analysis S/L/A/M did of nine simulation centers showed that they averaged 12,000 nsf (in a 20,000-sf floorplate) but the number was skewed by a few larger renovated facilities, says Olenick. Most new simulation centers are being built at 10,000 nsf.
In the clinical skills suite where students interact with “standardized patients” (trained actors playing the role of a patient), 12 exam rooms is the norm because certification tests require students to visit 12 rooms with different medical scenarios. These rooms are not used every day, however, so many institutions are adapting them to also function as simulation rooms, says Olenick.
In addition to clinical skills suites, simulation centers generally contain three to six simulation rooms of between 300 and 430 nsf. Those on the larger end accommodate ICU, NICU, and OR scenarios. Average exam rooms are around 130 nsf but are increasing to accommodate all the learners who need to be present and the experiences being simulated, says Olenick.
Net square footage per student for simulation center is getting more predictable, she adds, with a range between 70 and 100 nsf per medical student. When it comes to office space and staffing, the range goes from 800 to 2,600 nsf per person based on staffing space provided. Driving the disparity is the fact that programs and the staffing needed to support them are often just developing when the center is being designed, so office space provided is not necessarily reflective of final staffing levels. In addition, some centers dedicate space for research personnel, which can skew these ratios, says Olenick.
In its analysis, S/L/A/M found the office space benchmark fell into three groups: 750 to 1,000 nsf; 1,400 to 1,600 nsf; and 2,600 nsf per person.
“People tended to add staff later on, who then didn’t fit in the center and were put someplace else. We need to think about this variable more accurately when we do space programming or we will not meet operational needs,” she says.
Along with exams rooms and simulation areas is a third type of space—larger labs for individual or group training. Analysis of space utilization should take into account the varying lab and classroom time required by first-, second-, and third-year medical students, as well as capacity and availability of the rooms.
“We like people to consider designing exam rooms with excess capacity so they can flex into simulation rooms,” says Olenick. “Then we can take some of the demand and push it over into the exam rooms.”
Skills labs also can be designed to function as support space, like debriefing space, and can be designed for use as a simulation studio or a larger space for multiple events. “We need to cross over in these room uses to get the most value.”
Three Case Studies
In 2007, Emory University in Atlanta opened a new medical education building that included a state-of-the-art simulation center. The building ties together two historic campus buildings and an adjacent administration building for Emory Healthcare, explains Sidney Ward, a principal with The S/L/A/M Collaborative.
The layout necessitated the location of the skills labs on the lower level and the standardized patients suite on the third floor. The first and second floors are primarily lecture halls, classrooms, and small group rooms. “The design works well for Emory’s program, but separation of skills and simulation does cause challenges,” says Ward. A consolidated center allows for an economy of scale, flexible room use, and the ability to share staff resources and technology.
The lower level simulation suite contains a two-bay emergency room, a single patient room, an OR, an area for task trainers (models of various body parts used for skills practice), and a central multipurpose group room.
“The group room is a centralized flexible space with all of the simulation labs organized around it, including two adjacent debriefing rooms. This space is highly utilized and provides pre-event and debrief space, as well as overflow space for individual and group training. The quantity and location of debriefing rooms is one of the things that drives the amount of throughput these spaces can accommodate,” says Ward.
Adjacent to the simulation center are the gross anatomy lab and additional small group rooms. The small group rooms are driven by Emory’s problem-based learning curriculum, and are embedded throughout the facility.
“That adjacency allows them more flexibility and increased use of their simulation center. The other benefit of having the gross anatomy lab directly adjacent to the simulation labs is that, as gross anatomy needs change and require less space, the simulation lab can expand.”
Emory’s standardized patients area includes 16 exam rooms instead of the standard 12, because this module works better with the four societies it uses to subdivide each class.
“We probably wouldn’t include this number of exam rooms if we were starting from scratch and had a more flexible layout,” explains Ward. “One of the things we weren’t able to achieve was the separation of circulation between the learners and the standardized patients. But this space is some of the most flexible space they have in the building, and the students are drawn to it.”
Western Michigan University’s new School of Medicine, which accept its first class in early 2014, will accommodate a class size of 80 to 100. The facility is being built in an eight-story, 320,000-sf former Pfizer research building with a 30,000-sf, three-story addition for team-based lecture halls.
“WMU, in partnership with two local hospitals, will include a regional simulation center, so the scale is larger than what’s typical,” says Ward. “Incorporating an entirely new program into the 1970s-era building was challenging,” he adds.
The simulation lab and 12-exam room standardized patient suite are co-located on the ground floor, with a centralized control room adjacent. The center includes an OR, ER, patient rooms and flexible debriefing rooms. There are also two bioskills labs for task trainers and other individual and group activity.
Attributes that augment WMU’s regional and interprofessional missions include adjacent classrooms, diagnostic equipment, robotics, task trainer area, and a wet lab where they can make casts. “To reflect the continuum of care, a patient can come into an exam room, visit the emergency department, participate in an OR scenario, and go into recovery,” says Ward. There also is a nursing station and a pharmacy.
The square footage is almost twice as much as Emory’s because “it brings in all the pieces that make a regional center.”
Duke University’s previous simulation center was in a space about the same size as Emory’s. The new simulation center is on the fifth floor of Duke’s new medical education building with room for expansion on the floor above it.
The clinical skills exam area includes 12 exam rooms, two of which are a little bit larger so they can serve as patient rooms. The layout is the reverse of WMU, with the student write-up area centralized and the standardized patients’ access to the rooms along the exterior perimeter.
“It makes a really nice, open area, and flexible space that looks out across Duke’s campus,” says Ward.
Duke’s exam rooms are 120 sf, a smaller size that exactly models the exam rooms in Duke’s new clinical facility. “This slightly smaller footprint, along with the co-location of simulation and skills functions, enable the center to deliver more,” he adds. Flexible procedure and OR rooms have direct observation windows, and each room also has a moveable partition allowing it to be broken down into smaller areas. “That flexibility is helping to maximize the utilization out of roughly the same amount of square footage.”
The new center has resulted in Duke initiating a challenge called Duke Sim, to bring together people from across the institution to work collaboratively and develop inter-center simulation projects and maximize the simulation to improve education, research, and quality of care, says Grochowski.
“We are very focused on interprofessional education,” she says. “We can achieve that mission now that we have this facility and it is supported by this enterprise-wide initiative.”
Conclusions
Olenick offers three main points to remember when planning simulation centers:
- The simulation center will never be a profit center.
- Medical student education needs will drive the space program and design, but creative strategies can improve utilization and generate income.
- Consolidated simulation centers deliver the highest value.
“In the process of meeting your medical curriculum needs, you are building capacity for other opportunities, like interprofessional programs, professional development programs, and training programs with hospitals, or industrial partnerships,” she says.
“A consolidated simulation center, where the circulation spaces overlap, is probably going to deliver the most efficient and economical space. It will eliminate redundant spaces and reduce first costs. It will also reduce your operational costs, in that your staffing is going to be more efficiently addressed as well. That is something we would encourage.”
By Taitia Shelow
This report is based on a presentation Grochowski, Olenick, and Ward made at Tradeline’s Academic Medical and Health Science Centers 2013 conference.